Clinical
Case Report
Quantifying Muscle Compressibility as a New Decision Support
When pressure readings and clinical signs diverge.
Objective
Introduction
Conventional diagnostic criteria for compartment syndrome have shown limited reliability in capturing evolving tissue compromise. Recent studies reported that static pressure thresholds and one-time measurements provide limited diagnostic value, with substantial variability across techniques and poor correlation to actual tissue ischemia. Pressure readings alone are unreliable surrogate for microvascular compromise, and the classic “P” signs lack predictive accuracy. These findings reveal a gap between static pressure data and the dynamic state of tissue health [1,2], prompting the investigation into non-invasive alternatives for soft tissue assessment
Solution
Case Presentation
• A 40-year-old female sustained a displaced tibial plateau fracture (fig.1) with marked soft-tissue swelling, conferring ~50% ACS risk.
• Temporary stabilization was achieved using an external fixator.
• Continuous invasive Intracompartmental Pressure (ICP) monitoring was initiated.

Result
ICP Trend
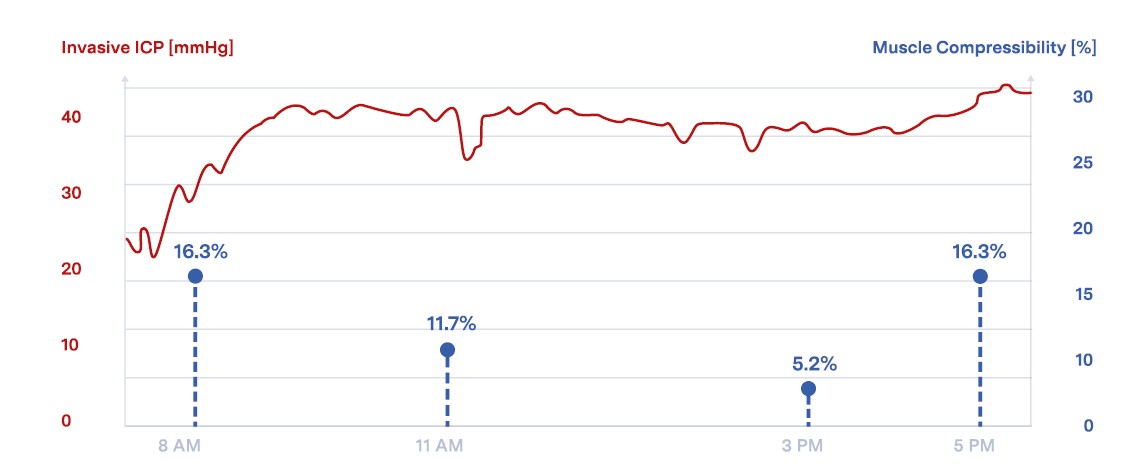
Initial pressure 30 mmHg, rising to 45 mmHg within 2 hours, remaining elevated for ~20 hours.
Clinical Status
ICP values were not correlated with the clinical examination. The patient showed no progressive pain, neurological deficit, or tense compartment.
Quantis ST Measurements
During this period, non invasive soft-tissue compressibility measurements were performed using Compremium Quantis® ST. Compressibility values dropped from 16.3% to 5.2% within 6 hours, followed by a recovery to the baseline of 16.3% after ~2 hours.
Outcome and conclusion
ICP remained high and stable throughout monitoring; treating doctors could not correlate the values with clinical findings. Reliance on ICP values alone would have indicated the need for prophylactic fasciotomy.
Compressibility measurements, however, exhibited a dynamic pattern with an initial decline followed by recovery to baseline, in alignement with the clinical assessment and patient aoutcomes.
This rebound in compressibility suggested restoration of tissue compliance, correlating with the absence of clinical deterioration.
Based on these findings, no prophylactic fasciotomy was performed.
The patient remained stable and achieved full functional recovery without complications.
This case was presented at OTA 2025 by Andrew H. Schmidt, MD Chief Orthopedic Surgery Hennepin Healthcare Minneapolis, MN, USA


